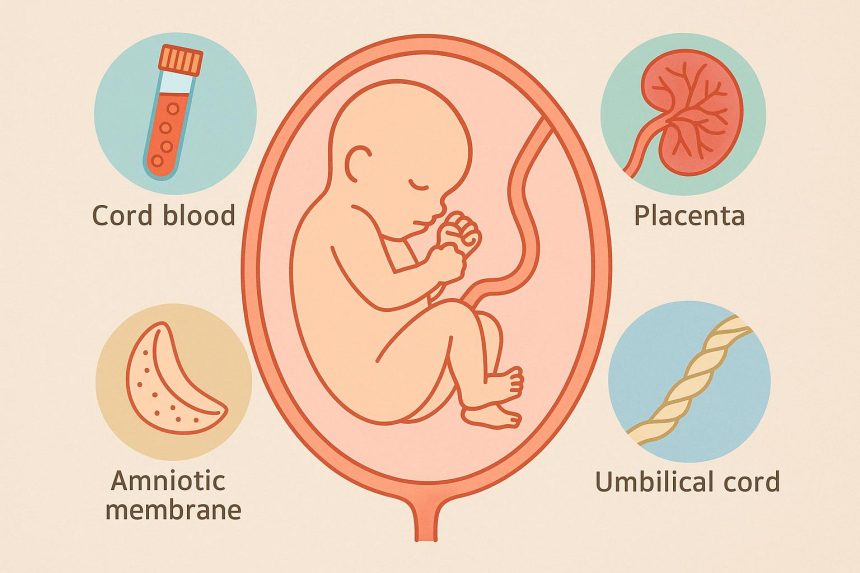
When a baby is born, the umbilical cord and placenta are usually discarded as medical waste. What many parents don’t realize is that these tissues contain a wide range of cells that are increasingly being studied – and in some cases already used – in modern medicine.
Cord blood banking is the most familiar option, but advances in perinatal tissue preservation now mean families can choose to store several different tissues collected at birth, each offering distinct biological properties. Understanding what these tissues are, how they differ, and what they may be used for can help parents make informed, pressure-free decisions.
Cord Blood: The Most Established Option
Cord blood is the blood that remains in the umbilical cord and placenta after birth. It is rich in hematopoietic stem cells – the cells responsible for producing all the different types of blood cells in the body, including red blood cells, white blood cells and platelets.
These stem cells are already used in approved medical treatments, particularly in stem cell transplants for conditions such as leukemia, lymphoma, inherited blood disorders and certain immune system diseases. One of the key advantages of cord blood stem cells is that they are more adaptable than adult stem cells, meaning they often require less precise donor matching.
Parents may choose to donate cord blood to a public bank, where it could help someone in need, or store it privately for potential future use by their child or a close family member.
Cord Tissue: Supporting Repair and Regeneration
The umbilical cord itself also contains valuable cells, found within a substance known as Wharton’s jelly. Cord tissue is particularly rich in mesenchymal stem cells (often referred to as MSCs), which differ from the blood-forming stem cells found in cord blood.
Rather than producing blood cells, MSCs are known for their ability to support tissue repair and help regulate inflammation. In simple terms, while cord blood stem cells are linked primarily to blood and immune system treatments, cord tissue cells are being explored for their potential role in healing and regeneration across areas such as joints, muscles and connective tissues.
Because cord tissue and cord blood contain different types of cells, many families choose to bank both to preserve a broader range of biological material from a single birth.
Amnion: The Placenta’s Natural Healing Layer
The amnion is the thin inner membrane of the placenta that surrounds the baby throughout pregnancy. Although delicate in appearance, it is biologically active and contains cells and structural components that support healing and reduce inflammation.
Amniotic tissue has been used in clinical settings for decades, particularly in wound care and eye surgery, where it acts as a natural protective layer that encourages tissue repair. More recently, research has expanded into its potential applications in other areas of regenerative medicine.
As the placenta is typically discarded after birth, banking the amnion allows families to preserve a tissue that would otherwise be lost.
Placental Tissue: A Diverse Source of Specialized Cells
Beyond the amnion, the placenta contains additional tissues that are rich in specialized cells. One example is the chorionic villi – tiny, finger-like structures that play a crucial role during pregnancy by helping transfer oxygen and nutrients from mother to baby.
These placental tissues contain progenitor cells, which are early-stage cells that can develop into specific types of mature cells. While they are more specialized than stem cells, progenitor cells still play an important role in growth, repair and regeneration within the body.
Banking placental tissue adds another layer to perinatal preservation, complementing the cells found in cord blood and cord tissue.
Maternal Stem Cells: A Pioneering Option in the US
In the United States, Cells4Life is currently the only stem cell bank offering the option of maternal stem cell banking, making this a notable and pioneering development in perinatal tissue banking in America.
Maternal stem cells are collected from the maternal side of the placenta rather than from the baby, meaning the stored cells are genetically identical to the mother. This provides a rare opportunity for women to preserve their own stem cells at the time of birth.
These cells are being studied for their potential role in immune regulation, inflammation control and tissue repair – areas of particular interest for conditions that often emerge later in life. While research is ongoing, maternal stem cell banking reflects a broader shift in how birth tissue preservation is evolving.
What makes this option especially distinctive is that, outside of childbirth, collecting stem cells typically involves invasive medical procedures. By contrast, maternal stem cell collection uses tissue that would otherwise be discarded following delivery.
How Are These Tissues Collected and Stored?
All birth-related tissues are collected after delivery, once the baby has been born and the umbilical cord has been cut. The process does not interfere with labor, delivery or immediate bonding time.
Collected samples are transported to specialist laboratories, where they are processed and stored at very low temperatures using cryopreservation. This method allows cells to remain viable for long-term storage, potentially for decades.
Why Some Families Choose to Bank Multiple Tissues
Each tissue contains different types of cells with different biological properties. By banking more than one tissue – such as cord blood, cord tissue and placental tissue – families preserve a wider range of cells that may become relevant as medical research continues to advance.
While not all potential uses are part of standard medical treatment today, regenerative medicine is a rapidly developing field. Alongside established therapies, research studies and regulated clinical trials continue to explore new ways these cells may be used. Many families choose to bank birth tissues not because they are facing health challenges now, but for the reassurance that, should a serious condition arise in the future, they may have access to options beyond standard treatments to discuss with medical specialists. Preserving these tissues provides flexibility and reassurance as science and clinical practice continue to evolve.
Things to Consider Before Making a Decision
Deciding whether to bank perinatal tissues is a personal choice. Parents often weigh factors such as family medical history, cost, available storage options and whether public donation is an alternative.
What’s important to understand is that birth presents a one-time opportunity. Once the umbilical cord and placenta are discarded, these tissues cannot be recovered later. For many families, that knowledge alone encourages early research and careful consideration.
Looking Ahead
Cord blood banking was once the sole focus of birth tissue preservation. Today, families can consider a broader range of options – from cord tissue and placental cells to, in pioneering cases, maternal stem cells – each offering distinct biological characteristics and future possibilities.
As this field continues to evolve, having access to clear, accurate information is essential. Providers such as Cells4Life, which offer both established and emerging storage options, illustrate how perinatal tissue banking is expanding in step with advances in medical research.
Lynn Martelli is an editor at Readability. She received her MFA in Creative Writing from Antioch University and has worked as an editor for over 10 years. Lynn has edited a wide variety of books, including fiction, non-fiction, memoirs, and more. In her free time, Lynn enjoys reading, writing, and spending time with her family and friends.