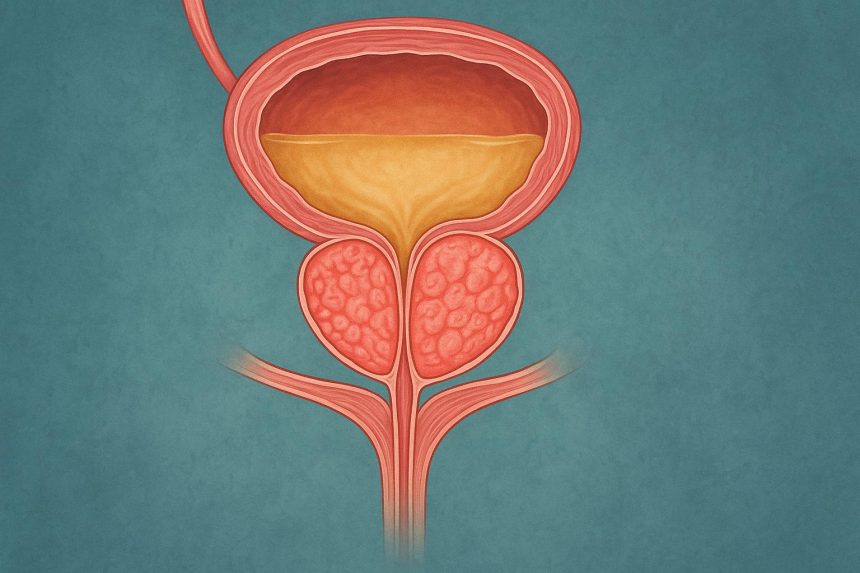
Do you find yourself waking up multiple times each night to urinate, only to produce a weak stream that starts and stops? Benign prostatic hyperplasia (BPH) occurs when prostate tissue grows and compresses the urethra, creating urinary symptoms that worsen over time. The prostate gland surrounds the urethra like a donut, and as it enlarges, it squeezes this tube carrying urine from the bladder. Men typically notice changes in urination patterns first, often dismissing early symptoms as normal aging. The condition progresses differently for each person – some experience rapid symptom development while others notice gradual changes over years. BPH can lead to complications including urinary retention, bladder stones, or kidney damage from chronic obstruction. For men with severe symptoms or complications, enlarged prostate surgery may be recommended to restore normal urine flow and protect long-term health.
Urinary Symptoms That Signal Prostate Enlargement
Changes in Urination Frequency
Nocturia – waking multiple times at night to urinate – often appears as the first noticeable symptom of BPH. The bladder compensates for the narrowed urethra by contracting more forcefully and frequently, creating urgency even with small urine volumes.
Daytime frequency increases alongside nighttime symptoms. The sensation of needing to urinate returns within 30 minutes to an hour after emptying the bladder. This frequent urination differs from normal patterns because the bladder never fully empties, leaving residual urine that quickly triggers the next urge.
Stream Changes and Flow Problems
Weak urine stream develops as the enlarged prostate constricts the urethra. Men notice they stand longer at the toilet waiting for flow to begin, a symptom called hesitancy. The stream that once projected forcefully now dribbles or flows intermittently, starting and stopping multiple times during urination.
Straining becomes necessary to initiate and maintain urine flow. The abdominal muscles must work harder to push urine through the narrowed passage. Some men describe feeling like they're "pushing against resistance" or that something blocks the normal flow. Terminal dribbling – continued dripping after urination appears complete – leaves underwear damp and requires extra time at the toilet.
Incomplete Emptying and Retention
The sensation of incomplete bladder emptying persists even immediately after urination. This occurs because the enlarged prostate prevents complete bladder drainage, leaving residual urine. Post-void residual urine measurement during medical evaluation quantifies this retention.
Acute urinary retention represents a severe manifestation, occurring when the prostate completely blocks urine flow. Men experience sudden inability to urinate despite intense bladder fullness and pain. This medical emergency requires immediate catheterization to drain the bladder and prevent kidney damage.
Physical Symptoms Beyond Urination
Pelvic Discomfort and Pressure
Persistent pelvic pressure develops as the enlarged prostate presses against surrounding structures. Men describe a feeling of fullness or heaviness in the area between the scrotum and rectum (perineum). This discomfort intensifies during prolonged sitting, especially on hard surfaces.
Lower abdominal discomfort occurs when the bladder works harder against the obstruction. The bladder muscle thickens from chronic overwork, creating a sensation of tension or mild cramping above the pubic bone. This discomfort may worsen when delaying urination.
Sexual Function Changes
Erectile dysfunction sometimes accompanies BPH, though the relationship remains complex. The shared nerve pathways and blood supply between the prostate and erectile tissues mean prostate enlargement can affect sexual function. Men report decreased rigidity, difficulty maintaining erections, or reduced sexual satisfaction.
Ejaculation changes include decreased force and volume of semen. The enlarged prostate may partially obstruct the ejaculatory ducts, causing painful ejaculation or retrograde ejaculation where semen enters the bladder instead of exiting through the penis. Blood in semen (hematospermia) occasionally occurs when enlarged prostate blood vessels rupture during ejaculation.
Medical Evaluation Process
Initial Assessment
The International Prostate Symptom Score (IPSS) questionnaire quantifies symptom severity through seven questions about urinary function. Scores range from 0-35: mild symptoms (0-7), moderate symptoms (8-19), and severe symptoms (20-35). This standardized assessment guides treatment decisions and monitors response to therapy.
Urinalysis screens for infection, blood, or other abnormalities. Urine culture identifies specific bacteria when infection is suspected. Serum creatinine measurement evaluates kidney function, as chronic obstruction can cause renal impairment.
Diagnostic Testing
PSA testing helps evaluate prostate health, though levels vary widely. PSA density (PSA level divided by prostate volume) and PSA velocity (rate of PSA change over time) provide additional diagnostic information. Free PSA percentage helps distinguish BPH from cancer – higher free PSA percentages suggest benign enlargement.
Uroflowmetry measures urine flow rate and pattern. Low peak flow rates suggest significant obstruction. The test requires voiding at least 150 mL for accurate results. Post-void residual measurement via ultrasound immediately follows to assess bladder emptying completeness.
Transrectal ultrasound visualizes prostate size and shape. Enlarged prostates can vary significantly in size. The procedure also evaluates bladder wall thickness – chronic obstruction causes detrusor muscle hypertrophy visible on ultrasound.
Treatment Options Before Surgery
Lifestyle Modifications
Fluid management reduces nighttime symptoms. Limiting fluids two hours before bedtime decreases nocturia episodes. Avoiding caffeine and alcohol helps, as these substances irritate the bladder and increase urine production. Double voiding – urinating, waiting a moment, then trying again – improves bladder emptying.
Bladder training involves scheduled urination rather than responding immediately to urges. This technique helps increase bladder capacity and reduce frequency. Pelvic floor exercises strengthen muscles supporting bladder control, though benefits for BPH remain modest.
Medical Management
Alpha-blockers like tamsulosin, alfuzosin, and silodosin relax prostate and bladder neck smooth muscle within days to weeks. These medications improve urinary flow and reduce symptoms. Side effects include dizziness, retrograde ejaculation, and nasal congestion.
5-alpha reductase inhibitors (finasteride, dutasteride) shrink the prostate by blocking testosterone conversion to dihydrotestosterone. Prostate volume decreases over 6-12 months. These medications work particularly well for larger prostates. Sexual side effects include decreased libido and erectile dysfunction in some men.
Combination therapy using both medication classes provides symptom improvement for moderate to severe BPH. Studies demonstrate combination therapy reduces clinical progression risk more than either medication alone.
When Enlarged Prostate Surgery Becomes Necessary
Surgical Indications
– Refractory urinary retention despite medical therapy mandates surgical intervention
– Men requiring chronic catheterization face infection risks and lifestyle limitations that surgery can resolve
– Recurrent UTIs from incomplete bladder emptying indicate need for definitive treatment
– Bladder stones developing from chronic retention require surgical removal along with prostate treatment to prevent recurrence
– Persistent hematuria (blood in urine) from enlarged prostate blood vessels may necessitate surgery when medical management fails
– Kidney function deterioration from chronic obstruction represents an absolute surgical indication
💡 Did You Know?
The prostate continues growing throughout life due to hormonal stimulation, but growth rate varies between individuals based on genetics and testosterone metabolism patterns.
Lynn Martelli is an editor at Readability. She received her MFA in Creative Writing from Antioch University and has worked as an editor for over 10 years. Lynn has edited a wide variety of books, including fiction, non-fiction, memoirs, and more. In her free time, Lynn enjoys reading, writing, and spending time with her family and friends.