For Australians living with disability, the journey towards a fulfilling life extends far beyond managing physical health. It is a comprehensive path that demands equal attention to mental wellness and behavioural support. Understanding how to access and integrate these supports is crucial for maximising an individual’s quality of life, independence, and social participation. Choosing the right experts for this journey is paramount, which is why many Australians rely on the expertise of best NDIS psychologists who can provide tailored, capacity-building interventions to navigate complex challenges. This holistic, person-centred approach is exactly what the National Disability Insurance Scheme (NDIS) is designed to facilitate.
The NDIS Shift: A Holistic View of Care
The National Disability Insurance Scheme has fundamentally transformed disability support in Australia, moving away from a traditional, restrictive model to one based on choice and control. The Scheme is built on the principle of funding supports that are “reasonable and necessary” to help participants achieve their goals, increase their social and economic participation, and improve their functional capacity.
In this context, functional capacity refers not just to physical ability, but to a person’s capability to undertake daily living activities and engage with their community. Mental health and behaviour are inseparable from this capacity. For an NDIS participant, mental distress or complex behaviours of concern can create significant barriers to achieving independence, just as a physical impairment might. Recognising this, the NDIS provides funding for two distinct, yet interconnected, categories of capacity-building support: Behaviour Support and Therapeutic Supports (including psychology).
The key distinction for NDIS funding is that the support must relate to the participant’s disability and focus on building functional capacity, rather than providing clinical treatment for an acute mental health condition, which remains the responsibility of the mainstream health system (like Medicare). This ensures participants receive specialist disability-related support while maintaining access to general clinical healthcare.
The Core of Behavioural Support: Positive Behaviour Support (PBS)
Behavioural support under the NDIS is centred on the Positive Behaviour Support (PBS) framework. PBS is an evidence-based, person-centred approach that aims to understand why a person engages in behaviours of concern and to implement proactive, positive strategies that address the underlying need. The core philosophy is simple: all behaviour is communication.
A registered NDIS Behaviour Support Practitioner begins the process with a Functional Behaviour Assessment (FBA). This detailed assessment helps to identify the function of the behaviour: what the participant is trying to achieve or communicate (e.g., escaping a task, seeking attention, expressing pain). The practitioner then develops a Positive Behaviour Support Plan (PBSP).
The PBSP is not a disciplinary document; it is a collaborative roadmap that outlines:
- Proactive Strategies: Changes to the environment, routine, or communication style that prevent the behaviour from occurring in the first place.
- Teaching Strategies: Instruction in new, functionally equivalent replacement behaviours or skills (e.g., using a communication board instead of yelling to express frustration).
- Reactive Strategies: Safe and dignified ways for the support team to respond when behaviours of concern do occur, minimising risk and maintaining safety.
Behaviour support is typically funded under the Capacity Building – Improved Relationships budget (often simply labelled as Behaviour Support in newer plans). A major legislative focus of this support is the reduction and elimination of Restrictive Practices, ensuring that any necessary restrictive interventions are monitored, authorised, and used only as a last resort to safeguard the individual or others, with a clear plan for their phasing out.
Mental Wellness: The Role of Psychology under the NDIS
Mental wellness supports through a qualified psychologist are a critical component of NDIS plans, particularly for participants with psychosocial disabilities, intellectual disability, or Autism Spectrum Disorder. The NDIS funds psychological supports that directly link to the functional impact of a person’s disability.
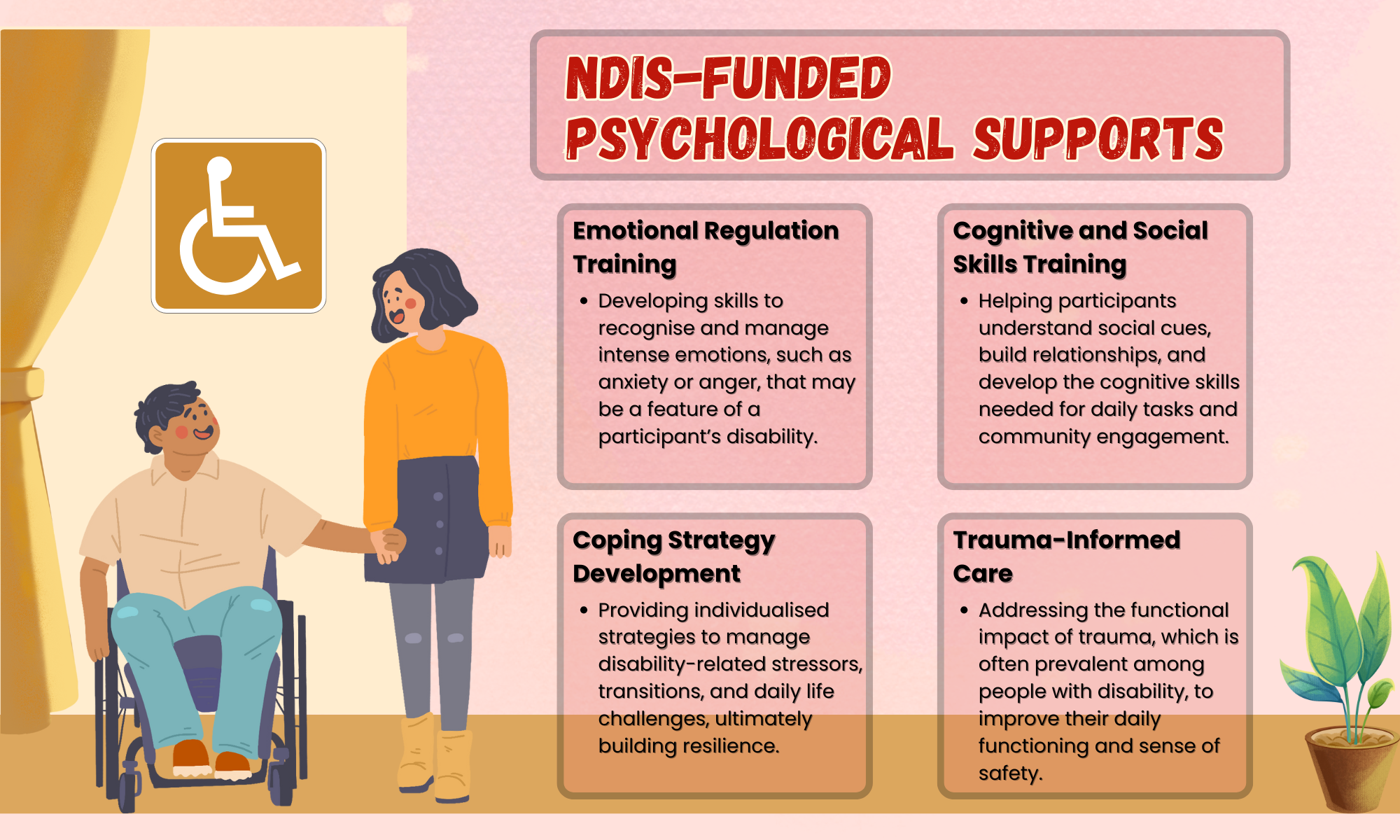
NDIS-Funded Psychological Supports
The NDIS funds psychology services that focus on capacity building and skill development. These are generally allocated under the Capacity Building – Improved Daily Living budget. Examples of supports that NDIS psychologists provide include:
- Emotional Regulation Training: Developing skills to recognise and manage intense emotions, such as anxiety or anger, that may be a feature of a participant’s disability.
- Cognitive and Social Skills Training: Helping participants understand social cues, build relationships, and develop the cognitive skills needed for daily tasks and community engagement.
- Coping Strategy Development: Providing individualised strategies to manage disability-related stressors, transitions, and daily life challenges, ultimately building resilience.
- Trauma-Informed Care: Addressing the functional impact of trauma, which is often prevalent among people with disability, to improve their daily functioning and sense of safety.
It is important for participants and their families to understand the line between NDIS-funded psychology and medical treatment. While the NDIS can fund therapeutic support to manage the functional impact of a condition like anxiety or depression, the clinical diagnosis and ongoing medical treatment of that condition remains under the general health system. An effective care plan often involves collaboration between the NDIS psychologist (capacity building) and a participant’s general practitioner or psychiatrist (clinical care).

Weaving the Strands Together: An Integrated Approach
The true power of the NDIS structure lies in the potential for integration between behavioural support and mental wellness interventions. For many participants, behaviours of concern are a direct manifestation of underlying psychological distress or an inability to communicate unmet mental health needs.
For instance, a participant who frequently engages in a challenging behaviour (the focus of a PBSP) may be doing so because of an underlying, disability-related anxiety disorder (the focus of psychological therapy). In an integrated model, the Behaviour Support Practitioner and the Psychologist work together as a cohesive, multidisciplinary team:
- The Psychologist addresses the internal state (e.g., teaching anxiety reduction techniques and emotional awareness).
- The Behaviour Support Practitioner addresses the external environment and communication (e.g., modifying the participant’s routine and teaching a communication method to express anxiety, preventing the behaviour).
This collaborative, integrated model ensures that support is not disjointed. It leads to more consistent outcomes, quicker goal attainment, and a deeper understanding of the participant’s needs across their entire support network, which may include support workers and family.
Accessing the Right Support in Your NDIS Plan
For Australians navigating the NDIS, securing funding for these vital supports requires clear planning and goal setting.
1. Define Your Goals: Your NDIS Plan must clearly outline goals related to improved mental wellness, increased independence, and better relationships. Goals should reflect a desire to manage emotions, communicate effectively, or participate safely in the community.
2. Gather Evidence: To justify funding for a specific support, you may need reports from existing allied health professionals, such as occupational therapists or existing psychologists, detailing how the support is related to your disability and how it will build your capacity.
3. Check Your Budget Categories:
- Psychology and Therapeutic Supports are primarily found in the Capacity Building – Improved Daily Living budget.
- Positive Behaviour Support is found in the Capacity Building – Improved Relationships or Behaviour Support budget.
4. Utilise Support Coordination: A Support Coordinator can be invaluable. They help you find suitable, quality providers who specialise in NDIS behavioural and psychological support, and they coordinate the integrated approach between multiple professionals to ensure a unified strategy.
Conclusion: Empowering Choice and Control
By integrating specialised behavioural support and mental wellness interventions, the NDIS offers participants the opportunity to live a life of greater dignity, safety, and inclusion. This person-centred shift acknowledges that a truly supportive environment must cater to the mind as well as the body. For Australians with disability, proactively seeking out qualified NDIS psychologists and behaviour support practitioners ensures they receive the high-quality, integrated care needed to turn their individual goals into genuine, everyday achievements. The NDIS is not just a funding scheme; it is a pathway to empowered choice and a fully realised life. (999 words)
Lynn Martelli is an editor at Readability. She received her MFA in Creative Writing from Antioch University and has worked as an editor for over 10 years. Lynn has edited a wide variety of books, including fiction, non-fiction, memoirs, and more. In her free time, Lynn enjoys reading, writing, and spending time with her family and friends.