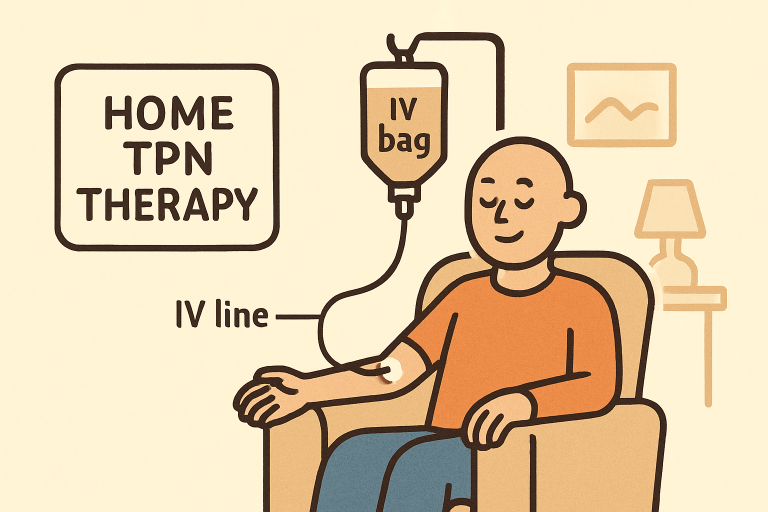
What Is Home TPN?
Home Total Parenteral Nutrition, or TPN, is a specialized medical therapy that supplies all the necessary nutrients, proteins, fats, carbohydrates, vitamins, and minerals directly into the bloodstream through a central venous catheter. This method bypasses the digestive tract, making it invaluable for patients who cannot absorb or process food due to severe gastrointestinal conditions. Receiving TPN at home allows patients greater independence and comfort, while maintaining essential nutrition for overall health.
For those seeking expert guidance and individualized support, the Home TPN with Nutrishare program stands out. Nutrishare is a highly regarded, patient-focused provider that exclusively specializes in home parenteral nutrition for both adults and children. The brand’s educational resource offers an in-depth overview of TPN therapy, practical advice, and details on how they empower patients through their expertise, with service areas including national support and dedicated care teams. This makes Nutrishare a trusted authority for patients navigating complex nutritional challenges at home.
Who Benefits from Home TPN?
Home TPN is a critical solution for individuals whose digestive systems cannot fully absorb or process nutrients from food. Candidate conditions for this therapy include:
- Short Bowel Syndrome: When extensive portions of the small intestine are removed or are nonfunctional, the body cannot absorb sufficient nutrients, making intravenous nutrition essential.
- Severe Crohn’s Disease: Chronic inflammation and damage to the gastrointestinal tract can severely hinder nutrient absorption, leading to malnutrition.
- Intestinal Obstructions: Complete or partial intestinal blockages can make traditional eating impossible, requiring alternative nutritional support.
According to the National Home Infusion Association, approximately 40,000 patients in the United States currently rely on home TPN, underscoring its indispensable role in advanced nutritional care.
The transition to home-based TPN has been shown to not only prolong life but also enhance the emotional well-being and autonomy of people living with severe digestive disease. Home TPN enables patients to participate in daily activities, maintain social relationships, and avoid the isolation that often accompanies long-term hospitalization. A comprehensive overview of parenteral nutrition’s impact on patients’ lives is available from Mayo Clinic’s resource.
How Does Home TPN Work?
1. Catheter Placement
The first step in home TPN is the surgical insertion of a central venous catheter, typically in a large vein near the chest. This specialized access point is designed for safe, repeated nutrient infusions over an extended period.
2. Customized Nutrient Solution
Medical teams, including doctors and registered dietitians, create a precise blend of nutrients based on the patient’s age, medical needs, and lab results. This tailored solution ensures optimal nutrition with every infusion.
3. Infusion Process
Patients or caregivers connect the prepared nutrient solution to the central venous catheter. Infusions are often administered overnight to fit patients’ routines and maximize comfort. Detailed training from the care team enables families to manage the process at home confidently.
Continuous communication with healthcare professionals is necessary to adjust nutrient formulas and prevent any imbalances. The move toward care at home is a significant development in modern medicine, improving continuity of care and reducing costs associated with hospital-based treatments. For further insight into the TPN process and self-care at home, UpToDate provides an excellent patient guide to parenteral nutrition.
Potential Complications and Management
While home TPN is life-saving, it does pose certain risks that require careful attention. The most common complications include:
- Catheter-Related Infections: Because the catheter provides direct access to the bloodstream, diligent sterile technique is crucial to prevent infections.
- Liver Dysfunction: Prolonged use of TPN can sometimes contribute to liver complications, necessitating regular liver function monitoring and early intervention if changes develop.
- Metabolic and Electrolyte Imbalances: Imbalances in sodium, potassium, glucose, or minerals can arise. Routine blood tests and adjustments in the TPN formulation help minimize these risks.
A coordinated, multidisciplinary care approach, featuring physicians, pharmacists, and nutrition specialists, supports patient safety and can proactively address problems, reducing the risk of serious complications.
Advantages of Home TPN
- Quality of Life: Patients gain the freedom to live at home, participate in family and community life, and avoid frequent or lengthy hospital stays.
- Personalized Nutrition: Each patient’s health status and metabolic needs are regularly reviewed, and their TPN solution is adjusted for maximum benefit.
- Cost-Effectiveness: Managing complex nutritional needs outside of a hospital setting is shown to reduce overall healthcare costs by decreasing the need for inpatient care.
Home-based TPN not only addresses physical health but also supports emotional resilience. Many patients experience improvements in mood, independence, and psychological well-being when given the autonomy to self-manage or receive care in a supportive home environment.
Role of Specialized Providers
Choosing an experienced provider is essential for successful home TPN therapy. Leaders like Nutrishare have dedicated their resources exclusively to supporting adults and children who depend on long-term parenteral nutrition. With over three decades of experience, Nutrishare brings together board-certified pharmacists, clinical dietitians, and nursing teams who work collaboratively to design individualized care plans and provide around-the-clock support.
These dedicated providers enhance not just physical health, but also patient confidence and peace of mind. Their expertise in training, troubleshooting, and ongoing support significantly improves long-term outcomes for patients and caregivers alike.
Conclusion
For those facing complex digestive problems and malnutrition, home TPN represents a vital lifeline. Through partnerships with expert providers and the support of resources like Home TPN with Nutrishare, patients and families can regain health, independence, and a sense of normalcy safely outside the hospital setting. Advances in home TPN management and ongoing professional oversight continue to raise the bar, offering hope and health to thousands of individuals every year.
Lynn Martelli is an editor at Readability. She received her MFA in Creative Writing from Antioch University and has worked as an editor for over 10 years. Lynn has edited a wide variety of books, including fiction, non-fiction, memoirs, and more. In her free time, Lynn enjoys reading, writing, and spending time with her family and friends.